Cytogenetics Lab: Clinical Applications
Advanced technology lab: For obstetrics or medical genetics patients, antenatal and postnatal testing.
Certain lymphomas & leukemias may be diagnosed with the use of oncological testing.
Prognosis and treatment regimens may be determined by doing oncological tests (including personalized targeted therapies).
For postnatal neurology & medical genetics patients, microarray DNA testing for constitutional abnormalities.
Technologies
A chromosomal breakage study may be used to detect Fanconi anemia, in addition to the conventional oncology & constitutional chromosome analysis.
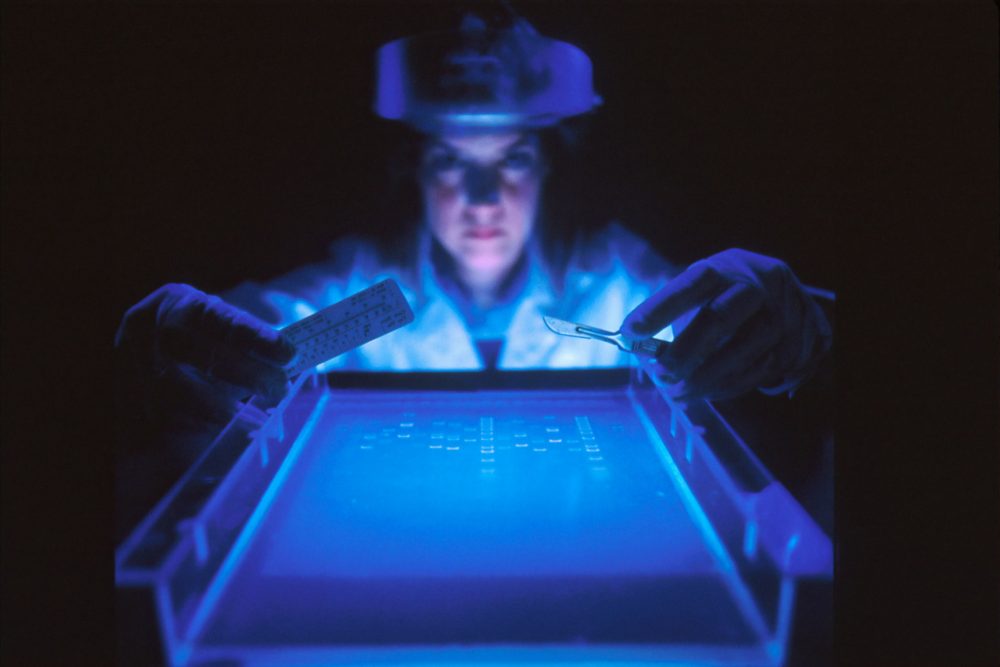
However, these assays are only some of the many fluorescence Intra situ hybridization (FISH) probes available.
For CLL, acute b-lymphoblastic leukemia (B-ALL), acute t-lymphoblastic leukemia, acute myeloid leukemia, MDS, and MM with plasma cell detection, there are comprehensive probe panels.
lymphoma of the mantle cell type:

In lung adenocarcinomas, ALK, RET, and ROS1 translocation and MET amplification are seen.
Other cancers of the fixed tissues
Screening for significant trisomies during pregnancy
Syndrome deletions and duplications in children
FISH for STAT situations that need rapid hybridization (four-hour TAT)
Physicians may use more than 44 available probes to identify deletions, duplications, rearrangements, and amplifications at the DNA level to help them diagnose and treat a wide spectrum of illnesses.
The American College of Medical Genetics recommends chromosomal genomic
The American College of Medical Genetics recommends chromosomal genomic ACGH as a first-tier test for people with non-syndromic developmental delay, intellectual disability, or autism spectrum disorder (ASD) phenotypic features because it allows a whole-genome survey at extremely high resolution to discover clinically relevant copy number abnormalities in those patients.
It is possible to identify sections of the microarray where there is no evidence of heterozygosity, which may have therapeutic implications for illnesses caused by uniparental disomy (UPD), identity by descent, or imprinting.
The Different Types Of Cytogenetic Testing: Advanced Technology Lab
Analyses Of Cytogenetics Or Karyotyping
This aids in the detection of chromosomal structure or numerical abnormalities. Cell cultures are required for chromosomal studies, which include the harvest of chromosomes, the banding of chromosomes, microscopic examination, and the generation of karyotypic samples.
Do cytogenetic tests have a place in the diagnostic process?
When a genetic anomaly is detected, cytogenetic testing is utilized.
High-Risk Pregnancies Need Prenatal Screenings.
Amniocentesis or chorionic villus sampling may be used to detect a fetus has aneuploidy, such as trisomy in Down syndrome, by cytogenetic testing.
Preliminary Examinations
If you’re looking for the root cause of developmental abnormalities or congenital anomalies, cytogenetic testing may be the answer. Diagnosis is a big comfort for the afflicted children’s families and enables them to get guidance on the best course of treatment and outlook.
Cancer Of The Blood And Blood Vessels
Chronic myeloid leukemia, for example, is diagnosed using cytogenetic testing because the Philadelphia chromosome, seen in around 95% of cases, is the product of a unique exchange of genetic material between chromosomes 22 and 9.
What Are The Cytogenetic Testing Contraindications?
Cytogenetic testing is safe and does not have any medical contraindications. Prior to conducting the tests, written permission should be acquired.
Do Cytogenetic Tests Have Any Advantages?
Diagnoses may be made via cytogenetic testing, as well as a long-term treatment. Additionally, genetic counseling for such a patient or his parents regarding the associated risk in either future pregnancies, and in certain situations, the geneticist’s decision to screen additional family members, is guided by this information.
 Is Cytogenetic Testing Good Or Bad?
Is Cytogenetic Testing Good Or Bad?
The resolution of cytogenetic testing is, however, limited. A variety of approaches may detect tiny gains and losses of genetic information, as well as bigger translocations, but they don’t enable testing even single nucleotide variants that might be linked to a patient’s health condition. In certain cases, cytogenetic testing may reveal chromosomal abnormalities that are not directly connected to the patient’s illness.
Molecular Cytogenetic Testing
Molecular Diagnostics Lab
To better understand illnesses, how they evolve, and how to best treat them in laboratory medicine was founded by the genetic revolution. Molecular diagnostics, which can now be performed in any size laboratory, is a real game-changer for the area of personalized medicine since it gives labs the ability to diagnose illness early and with more accuracy.
Most recently, automated platforms ( e.g. that produce precise findings using PCR method (PCR), as well as other molecular detection methods for identification or DNA/RNA quantification of infectious diseases, cancers, and human genes, have made molecular testing increasingly common. Since simpler, easier-to-use technologies save labor, even smaller laboratories are more interested in adding molecular capabilities. As molecular tests and tools become more straightforward, community hospital labs will be able to use them more widely. Hospital labs are also finding higher income prospects as a result of such new, more efficient methods.
Most importantly, labs may have a stronger influence on patient treatment and care by using molecular diagnostics. These cutting-edge devices aid doctors in the faster and more precise treatment of infectious illnesses. For instance, molecular or advanced technology labs are already having a positive impact on the virology lab. Culture-based testing, which was formerly the standard method for viral detection, is being replaced by molecular approaches for identifying viral infections. Patients will no longer have to wait two days or more for tests, which can put them at risk of missing out on vital therapy.
To diagnose respiratory infections, for example, PCR tests are employed instead of cultures. Medical professionals may employ molecular testing to detect diseases like RSV, rhinoviruses, as influenza A and B at an early stage, choose therapies, stop the spread of illness, and avoid overprescription of antibiotics.
As part of the hepatitis C treatment process, labs with molecular testing capability are essential. With the FDA’s approval of two new medications this year, doctors may use viral-load data to better treat this condition. For HCV, physicians are increasingly ordering molecular testing after a serological diagnosis. Antiviral medication may be started based on viral load measurements, which can also impact dose and treatment length choices and discover drug-resistant viruses. To keep tabs on the progress of treatment, frequent testing might be done. If the virus seems to be under control or completely eliminated, it will be proven by the fact that viral loads are well below the detection limit.
Monitoring using molecular diagnostic testing is also necessary for HIV patients on anti-viral drugs. A decrease in the HIV viral load is a key factor in the efficacy of antiviral medication therapy for HIV patients To establish if a patient is responsive to therapy, doctors use very sensitive molecular testing.
Clinical laboratories have also been thrust into the interesting and quickly developing area of customized medicine thanks to molecular technologies. Oncology patients are the principal benefactors of this trend thus far, since molecular diagnostic tests may identify individuals who are more likely to benefit from new cancer treatments. If a tumor is genetically susceptible to targeted, gene-based treatments, these tests notify doctors.
Herceptin targeted HER-2 and has saved countless lives since its introduction in 1998, maybe detected using the flag in situ hybrids (FISH) advanced technology lab in breast cancer patients who are most likely to benefit from therapy. The gene is present in one in four breast cancer patients. The laboratory plays a significant role in assisting oncologists in determining if a patient is a suitable candidate for Herceptin therapy based on genetic test findings.

Hemochromatosis Genotyping of the iron-overloading HFE gene
Carrier screening for cystic fibrosis patients
Detection of illness residuals (BCR/ABL1
HPV, CT/GC, and trichomoniasis are all diseases that affect women.
screening for Lynch syndrome (MSI, MLH1 methylation, BRAF)
Analysis of the total infectivity (CMV, EBV, adenovirus, HCV, HBV)
Genotyping of infectious agents
The Epi ProColon plasma test is used to detect colon cancer.
Panorama NIPT
It is also possible to identify HSV 1/2 in CSF and plasma samples using an ultrasensitive PCR technique. For both adult and pediatric bone marrow transplant programs, we provide comment engraftment monitoring tests.
According to the most recent NCCN recommendations, the laboratory is adopting customized cancer therapy and regularly updating our site-specific mutation panels (e.g. lung cancers, colon cancers, brain tumors, and hematologic malignancies).
Technologies
For our testing, we use cutting-edge technology that is only accessible to a clinical laboratory. Because of its involvement in clinical studies, the lab has had early access to cutting-edge advanced technology labs.
A wide variety of testing platforms are available, from basic to state-of-the-art.
Polymorphism in restriction fragment length
Accumulation by the use of a PCR
RT-PCR
Analysis of short tandem repeats using fluorescence
Automatic sequencing of genes using a capillary
Invader Hologic the PGM Illumina’s Panther Abbott M2000 PGM Illumina MiSeq Pyrosequencing
In-Depth Evaluation Procedures
Disorders inherited from a parent
Oncological and hematological tests
Monitoring of the smallest amounts of illness.
Diseases caused by infectious agents

Peripheral circulation of blood
Bone Marrow
Tissue obtained by autopsy
Urine
Fluid from the brain’s central nervous system
Cells that have been grown in culture
Stabilized tissues
PreservCyt cf DNA ThinPrep



 Is Cytogenetic Testing Good Or Bad?
Is Cytogenetic Testing Good Or Bad?